Background and objectives
Percutaneous laser disc decompression (PLDD) is a minimally invasive treatment option for vertebral disc herniation refractory to conservative treatment. PLDD was first used in 1986 and received approval from the U.S. Food and Drug Administration in 1991 (1). Based on the reduced risk associated with less invasive procedures, PLDD has increased in popularity, with reportedly over 30,000 PLDD procedures performed in 2001 (2). PLDD is performed under local anesthesia via a laser fiber percutaneously inserted into the nucleus pulposus. Laser energy is applied through the fiber, resulting in vaporization of nucleus pulposus contents (3).
Improvement in discogenic pain with PLDD is based upon laser-induced evaporation of water within the disc; this results in a very slight decrease in disc size due to water loss. Because the intervertebral disc is essentially a closed hydraulic system, a small decrease in volume leads to a significantly larger decrease of intradiscal pressure; in vitro experiments confirm this (4,5). The short term decrease in pressure is due to evaporation of water content within the nucleus pulposus; long term effects are thought to be due to protein denaturation, which limits the ability of the nucleus to resorb additional water and reduces stiffness of the disc (3,6,7). This hypothetically results in a more even distribution of weight across the intervertebral disc (8).
Consistent with a lumbar location for the majority of intervertebral disc herniations, most published studies have focused on the use of PLDD for the treatment of lumbar disc disease. Thoracic discogenic pain or herniation causing neural impingement is less common than that in the cervical or lumbar regions. Certain impact injuries, such as parachute landings, can result in thoracic disc damage. Invasive treatment of such injuries often involves a thoracotomy procedure with either a discectomy or fusion implantation. Although many studies have been done on lumbar and cervical PLDD procedures, few have been done on the thoracic region. In order to assess the efficacy and safety of PLDD for the treatment of thoracic disc disease, we performed a study of ten patients with thoracic discogenic pain who were unresponsive to conservative intervention.
Methods
We performed a prospective study of ten patients (8 male and 2 female) with an age range of 35-73 years. All patients presented with mid-thoracic axial (n=7) or radicular (n=1) pain that failed to improve with conservative management, which included typical modalities such as physical therapy, pain medication, and epidural steroid injections. Physical examination revealed localized thoracic pain without recreation of symptoms with palpation. The pain was either centralized or radiating to one side. There was no facet tenderness present. All the patients had negative facet injections, to evaluate for the possibility of facet joint pain as the underlying cause. The patients had positive discograms that correlated to their pain; in the case of the individual with radicular symptoms, she had total relief of her pain with a thoracic nerve root block, confirming this as the source of her pain. All patients were diagnosed with thoracic discogenic pain based on MRI and provocative discogram results. Magnetic resonance imaging (MRI) findings that were considered abnormal included changes described as irregular nuclear shape, reduced disc height, hypo-intense disc signal, annular tears, high intensity zones, endplate changes, and Modic changes (9,10,11).
All patients underwent diagnostic injections to confirm the source of their pain; these injections included either thoracic nerve root blocks for radicular symptoms and/or provocative discograms (12). The provocative discograms involved low-pressure injections of at least three disc levels and one of the levels was utilized as a control. Thoracic discography has been utilized as a controversial confirmatory test for discogenic pain for some time with debatable results (13,14). Studies show false positive results with discograms to be as high as 25% (13,15). A recent systematic review reported the published evidence to be of low quality (16). The authors identified only two studies by the same authors for inclusion, each over 10 years old. They recommended that other methods may be equally effective. Due to the lack of established accuracy of discography, we required the combination of an abnormal MRI and a positive provocative discogram to diagnose intervertebral discs as the source of pain and to identify potential study participants.
It was felt that gross herniations producing significant cord compression would be better treated with a laminotomy approach, and that not enough disc material would be removed to resolve the stenosis in such situations. Thus only patients with contained disc protrusions were considered for PLDD and patients with gross herniation were removed from the study and sent for laminotomy or conventional discectomy.
Patients' chosen for the procedure reported their thoracic pain using the Visual Analog Scale (VAS) pain scores at baseline. Posttreatment, patients were evaluated every six months via telephone call or direct patient contact for at least 18 months. The patient was specifically asked to address the pain level of the thoracic spine region and not the body as a whole. This was done to eliminate patients with short-term improvement from introducing bias. A double-blinded study would have been preferable with a sham group but was not possible at our facility.
The procedure begins with a properly prepped and draped patient in the prone position. All patients received intravenous (IV) antibiotics prior to the procedure. Cefofloxin was utilized unless there was an allergy, in which case ciprofloxin was used. Mild sedation was used during the procedure and the patient was able to converse with the surgeon in order to express any unusual pain. Sedation involved a combination of benzodiazepines and opiates. Fluoroscopy was utilized during the procedure for proper count of the thoracic vertebrae and to determine the entry site. The entry site was similar in position to a typical thoracic discogram and was approximately 3 inches lateral to the midline of the spine. Caution was necessary due to the lung fields being close to the needle entry site, increasing the risk of pneumothorax. Once the entry site was determined, the skin and deeper tissues were anesthetized with a mixture of 0.25% bupivacaine and 1% lidocaine with epinephrine via a 27-gauge needle. A 15 blade was used to create a stab incision of approximately ¼ inch. Through the incision, an 18-gauge, 3.5-inch spinal needle was inserted and the needle was guided into the middle of the disc using fluoroscopy. Positioning was confirmed via anterior and lateral x-ray views. Once properly placed, a direct firing holmium laser (diameter 0.5 mm) at 20 watts and 10 repetitions per second (6030-10405 Joules, mean 7633) was utilized in short bursts to vaporize the inside of the disc. In most cases these burst were of ten second intervals; the patient usually complained of burning mid back pain which limited the time per lasing period. After the lasing periods, the disc was “cooled” with normal saline (at least 100 ml) mixed with cefazolin (unless there was an allergy). Saline irrigation was performed after, not simultaneously with, laser application due to the size of the diameter of the working environment and because a running irrigant would reduce the laser's effectiveness and thus increase operating times. Total lasing time was approximately 3 minutes, but varied from 80 seconds to 300 seconds. In most cases, the end point was when the pressure in the disc was reduced and injection of the normal saline occurred without any resistance. At this point the needle was removed and either the next disc was commenced or the procedure was finished. Closure involved a single steri-strip over the incision. No sutures were used. Tegraderm and 2x2 gauze was placed over the wound.
Results
All ten patients tolerated the procedure well. There were no complications. Expected possible complications included those seen with thoracic discogram and laser usage such as infection or discitis, pneumothorax, nerve injury, and burn injuries (14). Each patient had a post procedural chest x-ray to rule out pneumothorax; no pneumothorax was seen. Length of follow-up ranged from 18 to 31 months (mean: 24.2 months). Patients were asked to assess their thoracic pain via a VAS score preoperatively and at final follow-up visit. Median VAS score pretreatment was 8.5 (range: 5-10) and median VAS at final follow-up was 3.8 (range: 0-9). Six of ten patients' scores improved by at least 6 points; one patient improved by 1 point and three patients' scores did not improve. No patients reported worsening of symptoms. Results are summarized in Table 1. No side effects were reported, and no adverse events occurred during the procedure.
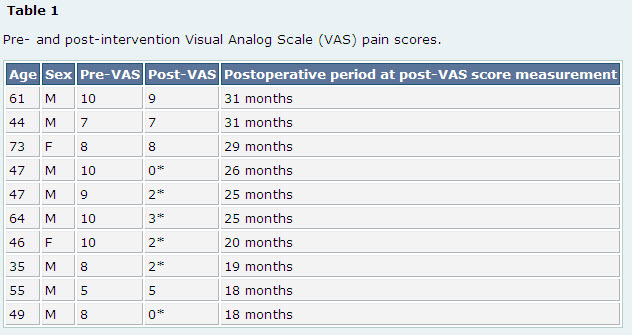
M: Male
F: Female
Pre-VAS: Visual Analog Scale pain score prior to PLDD.
Post-VAS: Visual Analog Scale pain score after PLDD.
*Patients (n=6, 60%) experiencing at least 6 point improvement in VAS postoperatively. Note that remaining patients reported minimal or no improvement.
Discussion
Thoracic disc disease is much less common than that of lumbar and cervical discs. However, certain types of impact, such as parachute landing, carry an increased risk of thoracic disc injury. Optimal treatment of thoracic discogenic pain is identical to that of disease of other spinal regions, i.e. aggressive medical management with anti-inflammatory medication, hot compresses, and physical therapy. Although epidural steroid injections are questionably proven to help with such cases, they are commonly utilized and are thus considered as a conservative therapy. Patients who fail to improve with conservative treatments have several invasive options, including conventional thoracotomy procedures for discectomy and fusion, posterior fusion, laminotomy, and disc decompression. These procedures generally carry significant risk and down time for potential patients.
Several different types of lasers are used when performing PLDD. High energy laser carriers the risk of tissue burns, but low energy lasers may be insufficient to adequately induce vaporization (1). Lasers near the infrared region currently used in PLDD include neodymium:ytrium-aluminum garnet laser [Nd:YAG], holmium:ytrium- aluminum-garnet laser [Ho:YAG], and diode laser. Lasers with visible green radiation include double-frequency Nd:YAG laser and potassium-titanyl-phosphate [KTP] laser. Most lasers use a 3mm outer cannula combined with a fiberoptic viewing cable (17). There is no clear consensus regarding the most effective and safe laser or the ideal wavelength that should be used (1). Most lasers provide 1200 Joules of energy in a pulsatile fashion (17).
PLDD is a minimally invasive technique that reduces intradiscal pressure by vaporization of a small volume of water within the nucleus pulposus. This results in decreased overall pressure and a more even distribution of weight across the disc, with subsequent relief of discogenic pain. PLDD is performed most commonly for lumbar disc disease, and published reports on the efficacy of PLDD in thoracic discogenic pain are lacking. The majority of PLDD studies are of small size and observational in nature; thus the true efficacy of this technique is uncertain (18). Multiple case series have reported success with PLDD for the treatment of lumbar discogenic pain (15,19-30); however, no randomized controlled trials have been performed. A systematic review by Singh et al. reported that conclusive evidence of efficacy is lacking, and large scale, comparative trials are warranted given the potential benefit of PLDD (18). The majority of authors report fair to good improvement in approximately 75% of patients, most commonly based upon the McNab scale. Immediate relief is reported to occur in 75-90% of patients. Rates of complication are low, the most common being septic or aseptic discitis, disc rupture, epidural hematoma, and nerve root damage (24,30-32).
A recent study on thoracic PLDD procedures by Hellinger et al. reported improvement in 41 of 42 patients six weeks after percutaneous laser decompression and nucleotomy (PLDN) (35). The authors reported three adverse events: one occurrence each of pneumothorax, pleurisy, and spondylodiscitis. Long-term outcome was not reported and thus it is unknown if their results extended beyond the study period of 6 weeks.
In our study, six of ten patients reported significant pain relief based on Visual Analog Scale pain scores concerning their thoracic pain issue. Utilizing a paired student's t-test, the differences between the pre- and post-treatment groups showed greater than a 99% confidence interval confirming that the improvement was indeed significant. The 60% improvement level noted is slightly lower, although still in agreement, with published reports of PLDD in patients with lumbar disc disease (15,19,34). Of interest, patients appeared to fall into two main groups: those gaining significant improvement and those receiving little or no improvement at all. In reviewing the patients who failed treatment, we could not distinguish any specific features, such as MRI findings or other clinical data, which could be utilized to screen these potential failed patients in the future.
Importantly, no adverse events occurred in the intra- or postoperative period. Intervention for the treatment of thoracic disc disease carries a risk of pneumothorax, and particular concern was given to this possibility during the intervention. No patient developed pneumothorax, and no evidence of discitis, infection, or nerve injury was noted.
Conclusion
This is one of the first reports of the successful application of PLDD for the treatment of thoracic discogenic pain. Although the study group is small with only ten patients, six out of the ten patients reported significant improvement at long-term (greater than 18 month) follow-up, and no adverse events were reported. PLDD could be considered a viable option with a low risk of complication for the treatment of thoracic discogenic pain that does not resolve with conservative treatment. Nonetheless, due to the small study size, we recommend a larger double-blinded study to confirm our results.